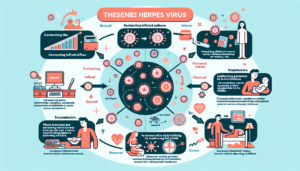
We’ve all heard of herpes, but did you know that there are actually two types: HSV-1 and HSV-2? These two strains of the virus may sound similar, but they actually have some key differences. HSV-1 is commonly known as oral herpes and usually causes cold sores around the mouth, while HSV-2, also known as genital herpes, is primarily transmitted through sexual contact. In this article, we’ll explore the nuances between these two types of herpes, helping you gain a better understanding of their differences and how they can affect your health. So, let’s dive in and unravel the mystery behind HSV-1 and HSV-2!

HSV-1 vs. HSV-2
Herpes simplex virus (HSV) is a common viral infection that affects millions of people worldwide. There are two types of HSV: HSV-1 and HSV-2. While they may sound similar, they have some important differences. In this article, we will explore the transmission, prevalence, symptoms, recurrence, complications, diagnosis, treatment, prevention, and misconceptions surrounding HSV-1 and HSV-2.

Transmission
Oral Transmission
HSV-1 is primarily transmitted through oral contact, such as kissing or sharing utensils. It is commonly associated with oral herpes, which manifests as cold sores or fever blisters on or around the mouth. HSV-1 can also be transmitted to the genitals through oral-genital contact, although this is less common.
Genital Transmission
HSV-2, on the other hand, is mainly transmitted through sexual contact. It is commonly associated with genital herpes, which causes painful sores or blisters on or around the genitals. HSV-2 is highly contagious during outbreaks, but it can also be transmitted when there are no visible symptoms.
Prevalence
Global Prevalence
Both HSV-1 and HSV-2 have high prevalence rates globally. It is estimated that over half a billion people worldwide are infected with HSV-1, while around 290 million people are infected with HSV-2. These infections are more common in developing countries with limited access to healthcare and education.
Regional Prevalence
The prevalence of HSV-1 and HSV-2 varies across different regions. HSV-1 infections are more prevalent in Asia, Africa, and South America, whereas HSV-2 infections are more common in North America, Europe, and Australia. However, it is important to note that these trends are not exclusive, and both types of HSV can be found worldwide.
Symptoms
Oral Symptoms
HSV-1 infections typically manifest as cold sores or fever blisters on or around the mouth. These sores are often painful, and they may crust over before healing. Some individuals may experience flu-like symptoms during the initial outbreak, including fever, headache, and fatigue. It is important to note that many people infected with HSV-1 may not experience any symptoms at all.
Genital Symptoms
HSV-2 infections primarily affect the genital area. The symptoms include painful genital sores or ulcers, itching, and a burning sensation during urination. Like HSV-1, some individuals may also experience flu-like symptoms during the initial outbreak. It is essential to seek medical attention if you suspect genital herpes, as proper diagnosis and management are crucial.
Recurrence
Frequency
Both HSV-1 and HSV-2 infections are characterized by periods of recurrence. After the initial outbreak, the virus remains dormant in the body and can reactivate periodically, causing new symptoms. The frequency of recurrences varies from person to person, with some individuals experiencing outbreaks several times a year, while others may only have occasional or rare recurrences.
Triggers
Several factors can trigger the reactivation of HSV, leading to recurrent outbreaks. These triggers may include stress, exposure to sunlight, hormonal changes, weakened immune system, and certain medications. By identifying and avoiding these triggers, you may be able to reduce the frequency and severity of recurrent outbreaks.

Get 51% Discount If You Order Now!
Complications
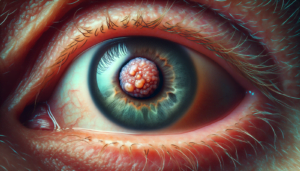
Oral Complications
While HSV-1 infections are generally considered less severe than HSV-2 infections, they can still lead to complications. In some cases, the virus can spread to the eyes, causing a condition called ocular herpes. Ocular herpes can lead to eye pain, redness, blurred vision, and even vision loss if left untreated. It is important to seek professional medical care if you suspect ocular herpes.
Genital Complications
HSV-2 infections can pose more significant complications, particularly during pregnancy. If a pregnant individual has an active genital herpes outbreak near the time of delivery, there is a risk of transmitting the virus to the baby, which can lead to severe infections and potentially lifelong health issues. Therefore, it is vital to inform your healthcare provider if you have a history of genital herpes during pregnancy.
Diagnosis
Physical Examination
Doctors can often diagnose HSV based on a visual examination of the sores or lesions. They will look for characteristic symptoms and signs, such as the appearance of the sores, their location, and other associated symptoms. However, a physical examination alone cannot determine the type of HSV, so additional tests may be necessary.
Laboratory Tests
Laboratory tests, such as polymerase chain reaction (PCR) or viral culture, can confirm the presence of HSV and distinguish between HSV-1 and HSV-2. These tests involve taking samples from the sores or lesions and analyzing them in a laboratory. Blood tests can also detect HSV antibodies, which indicate a previous or current infection.
Treatment
Antiviral Medications
Antiviral medications are commonly prescribed to manage HSV infections. These medications, such as acyclovir or valacyclovir, can help reduce the severity and duration of outbreaks, as well as decrease the risk of transmitting the virus to others. They are most effective when taken at the first sign of an outbreak or during prodromal symptoms.
Home Remedies
In addition to antiviral medications, various home remedies can help alleviate symptoms and promote healing. Applying ice packs or cold compresses to the affected area can help reduce pain and swelling. Maintaining good hygiene, keeping the affected area clean and dry, and wearing loose-fitting clothing can also aid in the healing process.
Prevention
Safe Sexual Practices
Practicing safe sex, such as using condoms consistently and correctly, can significantly reduce the risk of HSV transmission. However, it is important to note that condoms may not provide complete protection, as HSV can be transmitted through skin-to-skin contact in areas not covered by a condom.
Avoiding Direct Contact
Avoiding direct contact with active sores or lesions is crucial in preventing HSV transmission. If you or your partner is experiencing an outbreak, it is best to abstain from any sexual activity until the sores have completely healed. It is also important to refrain from sharing personal items, like towels or razors, that may come into contact with the affected area.
Vaccination
Currently, there is no vaccine available for HSV-1 or HSV-2. However, ongoing research and clinical trials are exploring the development of vaccines to prevent or reduce the severity of HSV infections. It is essential to stay updated on the progress of these vaccines and consult with healthcare professionals for the latest recommendations.
Misconceptions
Cold Sores vs. Herpes
Cold sores, also known as fever blisters, are usually caused by HSV-1. While cold sores are a form of herpes, they should not be confused with genital herpes caused by HSV-2. The location and mode of transmission differ between these two types of herpes, but both can cause discomfort and require appropriate management.
HSV-1 as a Non-Sexually Transmitted Condition
Contrary to popular belief, HSV-1 can be transmitted sexually, although it is predominantly associated with oral herpes. Engaging in oral-genital contact can lead to the transmission of HSV-1 to the genitals. It is important to practice safe sex and have open communication with partners to prevent the spread of both HSV-1 and HSV-2.
In conclusion, understanding the differences between HSV-1 and HSV-2 is crucial for prevention, diagnosis, and management. While the two types of herpes share some similarities, such as recurrent outbreaks and the potential for complications, their modes of transmission differ significantly. By practicing safe sex, maintaining good hygiene, and seeking medical attention when necessary, you can take control of your health and reduce the impact of HSV infections. Remember to consult with healthcare professionals for personalized advice and guidance.