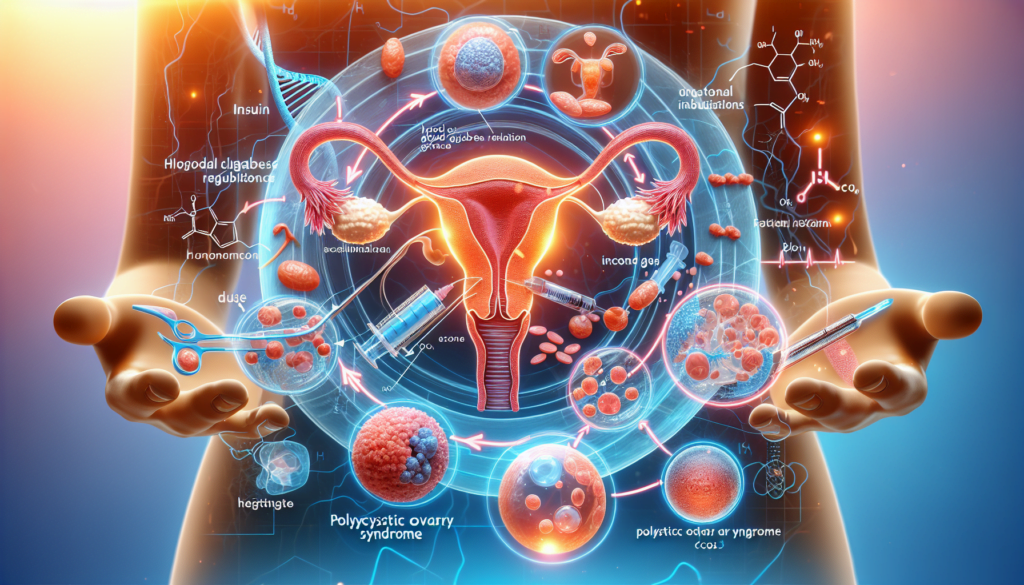
You’ve probably heard of PCOS (Polycystic Ovary Syndrome) before, but did you know that it is often linked to insulin resistance? Insulin resistance is a condition where the body’s cells don’t respond properly to insulin, leading to high blood sugar levels. When insulin resistance is present in women with PCOS, it can cause a range of hormonal imbalances and unwanted symptoms. In this article, we will explore the connection between insulin resistance and PCOS, and discuss the potential impacts it can have on women’s health. So, grab a cup of tea and get ready to learn more about this fascinating link!
What is PCOS?
Definition
Polycystic ovary syndrome (PCOS) is a hormonal disorder commonly experienced by women of reproductive age. It is characterized by imbalances in reproductive hormones, resulting in various symptoms and potential complications.
Causes
The exact cause of PCOS is still unknown, but it is believed to be influenced by a combination of genetic and environmental factors. Hormonal imbalances, insulin resistance, and inflammation are believed to play a significant role in the development of PCOS.
Symptoms
PCOS can manifest differently in different individuals. Some common symptoms include irregular periods, excessive hair growth (hirsutism), acne, weight gain, and difficulty getting pregnant. However, it is important to note that not all women with PCOS experience the same symptoms, and the severity of symptoms can vary.
Insulin Resistance and PCOS
Understanding Insulin Resistance
Insulin resistance is a condition in which the body’s cells become less responsive to the hormone insulin. Insulin plays a crucial role in regulating blood sugar levels. When the cells become resistant to insulin, it leads to an accumulation of glucose in the bloodstream, causing higher insulin levels. This condition can eventually lead to the development of type 2 diabetes.
The Link between Insulin Resistance and PCOS
Insulin resistance is closely associated with PCOS. Many women with PCOS have been found to have insulin resistance as well. The exact relationship between the two conditions is still being studied, but it is believed that insulin resistance can contribute to hormonal imbalances and the development of PCOS symptoms.
Effects of Insulin Resistance on PCOS
Hormonal Imbalance
Insulin resistance can disrupt the delicate balance of reproductive hormones in the body. This can result in elevated levels of testosterone, leading to symptoms such as hirsutism and acne. Hormonal imbalances can also affect the regularity of menstrual cycles and interfere with ovulation.
Ovarian Dysfunction
Insulin resistance can also impact the normal functioning of the ovaries. It can disrupt the maturation of eggs and the release of mature eggs during ovulation. This can contribute to infertility and difficulties in conceiving.
Fertility Issues
Infertility is a common concern for women with PCOS. The combination of hormonal imbalances and ovarian dysfunction caused by insulin resistance can make it more challenging to achieve and maintain a pregnancy. Proper management of insulin resistance is crucial in addressing fertility issues associated with PCOS.

Diagnosing Insulin Resistance in PCOS
Medical History and Physical Examination
Diagnosing insulin resistance in PCOS typically involves a thorough medical history review and a physical examination. Your healthcare provider may ask about your menstrual history, symptoms, and family history of PCOS. They may also perform a physical examination to check for signs of insulin resistance, such as excess body weight and skin changes.
Blood Tests
Blood tests can provide valuable information to diagnose insulin resistance. Fasting glucose and insulin levels, as well as a glucose tolerance test, can help determine the body’s ability to handle glucose and insulin. Additionally, other hormone levels may be measured to assess the overall hormonal profile.
Other Diagnostic Procedures
In some cases, additional diagnostic procedures may be performed to evaluate insulin resistance in PCOS. These may include imaging tests like ultrasound to assess the ovaries and rule out other potential causes of symptoms.
Managing Insulin Resistance in PCOS
Lifestyle Modifications
Lifestyle modifications are often the first line of defense in managing insulin resistance in PCOS. These typically involve dietary changes, regular physical activity, and weight management. A balanced diet with a focus on low glycemic index foods and adequate fiber intake can help stabilize blood sugar levels. Regular exercise has been shown to improve insulin sensitivity and promote weight loss, further aiding in managing insulin resistance.
Medications and Supplements
In some cases, lifestyle modifications alone may not be sufficient to manage insulin resistance in PCOS. Medications and supplements can be prescribed to improve insulin sensitivity and regulate hormonal imbalances. Commonly prescribed medications include metformin, which helps reduce insulin levels, and thiazolidinediones, which improve the body’s response to insulin. Supplements like inositol, methylcobalamin, vitamin D, and omega-3 fatty acids may also be recommended to support insulin metabolism and overall health.
Dietary Approaches for Insulin Resistance and PCOS
Low Glycemic Index Diet
A low glycemic index (GI) diet focuses on consuming carbohydrates that have a minimal impact on blood sugar levels. Foods with a high GI quickly raise blood sugar levels, while low GI foods are digested more slowly, resulting in a steadier release of glucose into the bloodstream. By choosing lower GI foods, individuals with PCOS can help maintain stable blood sugar levels, manage insulin resistance, and prevent sudden spikes and drops in blood sugar.
Balanced Macronutrients
A balanced macronutrient intake is essential for managing insulin resistance in PCOS. This means including a combination of carbohydrates, proteins, and fats in each meal. Balancing the intake of these macronutrients can help regulate blood sugar levels and promote a more stable insulin response.
Importance of Fiber
Fiber is an essential component of a PCOS-friendly diet. It helps slow down the digestion and absorption of glucose, preventing rapid spikes in blood sugar levels. Additionally, fiber aids in regulating bowel movements, promoting digestive health, and supporting weight management, which can all positively impact insulin resistance.
Exercise and Insulin Resistance in PCOS
Benefits of Regular Exercise
Regular exercise offers numerous benefits for individuals with PCOS and insulin resistance. It helps improve insulin sensitivity, allowing the body’s cells to better respond to insulin. Exercise also aids in weight management, reduces inflammation, and enhances overall cardiovascular health.
Recommended Exercise Types and Intensity
A combination of aerobic exercise (such as brisk walking, cycling, or swimming) and strength training is recommended for managing insulin resistance in PCOS. Aim for at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous aerobic exercise per week. Strength training exercises should be performed at least twice a week to promote muscle health.
Medications for Insulin Resistance in PCOS
Metformin
Metformin is a medication commonly prescribed to individuals with PCOS and insulin resistance. It works by reducing the liver’s production of glucose and increasing the body’s sensitivity to insulin. Metformin can help regulate menstrual cycles, lower insulin levels, and manage weight in individuals with PCOS.
Inositol
Inositol is a naturally occurring compound that has been shown to improve insulin sensitivity in women with PCOS. It can help regulate menstrual cycles and improve fertility by restoring hormonal balance. Inositol supplements are available in different forms, such as myo-inositol and D-chiro-inositol.
Thiazolidinediones
Thiazolidinediones are another class of medications used to improve insulin sensitivity in PCOS. They work by increasing the uptake of glucose by the body’s cells and reducing insulin resistance. These medications are typically prescribed in specific cases and should be used under the guidance of a healthcare professional.
Supplements for Insulin Resistance in PCOS
Methylcobalamin
Methylcobalamin, a form of vitamin B12, has been shown to have beneficial effects on insulin resistance in PCOS. It helps improve insulin sensitivity and may aid in reducing insulin resistance-related symptoms. Supplementation with methylcobalamin should be done under medical supervision.
Vitamin D
Vitamin D deficiency is common in individuals with PCOS and may contribute to insulin resistance. Supplementation with vitamin D, alongside regular exposure to sunlight, can help improve insulin sensitivity and overall health in women with PCOS.
Omega-3 Fatty Acids
Omega-3 fatty acids have anti-inflammatory properties and may help reduce insulin resistance and improve hormonal imbalances in PCOS. Incorporating dietary sources of omega-3 fatty acids, such as fatty fish or flaxseeds, or taking fish oil supplements can be beneficial.
Conclusion
Importance of Managing Insulin Resistance in PCOS
Managing insulin resistance is crucial for individuals with PCOS to alleviate symptoms, regulate hormonal imbalances, and promote overall health and well-being. By addressing insulin resistance through lifestyle modifications, medications, and supplements, women with PCOS can improve their fertility, reduce the risk of complications, and enhance their quality of life.
Seeking Professional Help
If you suspect you have PCOS or have been diagnosed with it, it is important to seek professional help from a healthcare provider with experience in treating PCOS. They can help diagnose insulin resistance, develop a personalized treatment plan, and monitor your progress to ensure the most effective management of your condition. Remember, you don’t have to face it alone. Help is available to support you on your journey towards better health.


